15th International Symposium on Pediatric Neuro-Oncology
International Symposium on Pediatric Neuro-Oncology (ISPNO) June 24 – 27, 2012, Family Day
The Childhood Brain Tumor Foundation was delighted to provide a Silver Sponsorship for the 15th ISPNO and supported the Nursing Symposium.
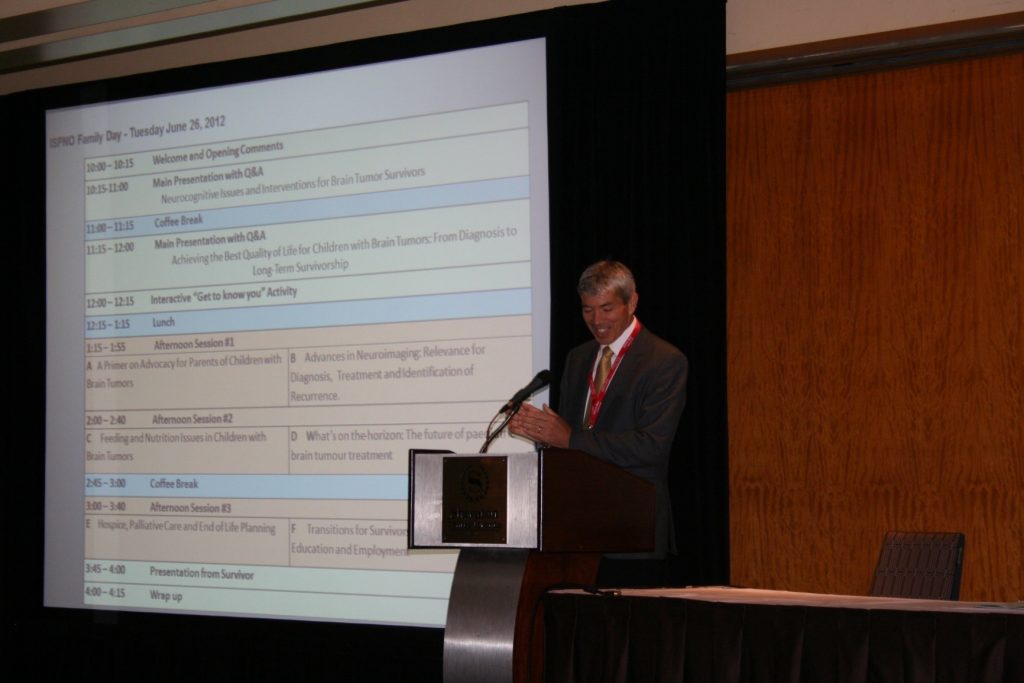
The ISPNO also included a special day organized to provide an educational opportunity for families on Tuesday, June 26, 2012. Nearly 75 parents and children attended. Medical professionals provided detailed information about a variety of important topics. Families had an opportunity to socialize with one another.

This summary will cover a portion of several presentations that were given. Dr. Eric Bouffet warmly welcomed the families who were in attendance and referenced the agenda and the topics to be covered.
An introduction for the first morning speaker was given by Dr. Laura Janson, Hospital for Sick Children, Toronto. She and Dr. Kristina Hardy, Children’s National, Washington, DC presented “Neurocognitive Issues and Interventions for Brain Tumor Survivors.” Dr. Janson provided an overview of an ongoing research/intervention program related to memory. The study involved the following focus areas: 1.) Changes in learning and memory after treatment, 2.) Why we think changes occur, and 3.) What has been done to help survivors?
Neurocognitive Issues and Interventions for Brain Tumor Survivors, presented by Lauren Jansen, Ph.D., Hospital for Sick Children and Kristina Hardy, Ph.D., Children’s National, Washington, DC. Brain tumor survivors often have neurocognitive late effects that may include changes in learning and memory near the completion of treatment. Children may experience trouble learning new material, forget what they have learned, or learn more slowly due to slower processing speed. Attention issues may also play role. Poor academic achievement in mathematics calculations, reading comprehension, handwriting, and inability to finish work under timed conditions are often a concern. The risk factors are often more significant for females, as they are more likely to develop cognitive changes and other late effects. In addition, younger age at diagnosis may be predictive of later problems. Other factors include tumor location, whether the child had hydrocephalus, treatments, such as radiation to the brain, and surgery. Genetics are strongly suspected to play a role, but there is less data regarding genetic influence at this time.
The brain’s white matter is made up of special brain cells that are responsible for the brain’s communication network. This network develops rapidly in youth and allows information to move from one place to another. Children still develop white matter through their teens. Evidence has shown that radiation and chemotherapy have an effect on white matter and can make it difficult for the brain tumor carry signals as effectively. Damage is attributed to small damage to blood vessels of the brain.
Concerns related to executive function include slowed processing speed, memory (verbal and nonverbal), and difficulty with planning and organizing. Some children may experience problems generating novel ideas or solutions that apply to their studies. Executive function also includes attention, behavior regulation, flexibility in problem solving, and emotional control; some of which may be impacted in survivors. It is very important for children undergoing treatment for their brain tumor to have an early baseline assessment with a neuropsychologist to ensure changes can be tracked. Close monitoring and evaluations over time are needed.
Accommodations may be made through educational support and may include: breaking down material in small steps, preferential seating, time management, keyboarding, reduced workload, or additional time for testing and other accommodations as needed depending on the specific need. Children with hearing, vision, or motor losses may require additional accommodations. It is vital that parents engage with the educational professionals and help drive the changes in an appropriate manner. In some cases children may require stimulant medication, such as, Ritalin, Concerta, or a new medication, modafinil (Provigil ®), and analeptic drug used to treat narcolepsy. Studies have shown that Omega-3 fatty acids may be potentially effective. Stimulant medications increase attention span, processing speed and short term memory, but there are only minimal gains associated with academics.
Cognitive Remediation or Neurorehabilitation
Cognitive remediation is a means of adapting strategies to help individuals who have experienced brain injury to recover some basic function. Randomized clinical trials were conducted by Dr. Hardy and were based on elements of traditional rehabilitation. Treatment was intense and involving two hours a week for six months. Sixty percent of participants completed the program and gained achievements in attention, memory, improved writing, and social skills. The 40% of survivors that did not complete the program may have had difficulty with the program intensity or coming to clinic logistically may have been prohibitive. A home-based model was considered to have an advantage. Through a home-based approach participants could reduce the number of clinic visits, practice targeted skills with greater intensity, and use a coaching system via telephone. Children seem receptive to the “video game” format, especially at a younger age. The pilot program Captain’s Log, Brain Train, did not have a fixed training period, but suggested training for 60 minutes, three to four times a week. An analogy was given that brain rehabilitation could be equated with exercise, something to increase for greater benefit.
In summary, through the pilot program, half of the participants saw improvement in working memory over three months. Those that trained the most showed the greater improvement. According to parents, greater improvement in working memory skills occurred after training intervention.
Several pilot programs that could influence cognitive rehabilitation include: Captain’s Log, Brain Train, CogMed (cogmed.com), TRICCS, and Luminosity (can be successful in adolescents). Many of these programs are currently being assessed. Questions arose from the audience regarding programs suitable for participants with hearing deficits or other sensory losses. Brain Train has an auditory component for the visually impaired. CogMed has a coaching program that may be beneficial.
Achieving the Best Quality of Life for Children with Brain Tumors: From Diagnosis to Long-term Survivorship, presented by Dr. Stewart Goldman, Children’s Memorial, Chicago, IL

“Cost of the cure has a lifetime to be repaid.” Dr. Goldman stated that we are treating the child not the tumor and further commented that statistics are good to hear once, but reminded the audience that every child is an individual. He stressed that the multi-disciplinary team approach to treating children with brain tumors is optimal. Dr. Goldman encouraged parents/survivors to take notes during meetings and write questions down because approximately only 5 to 10% of an initial discussion can be retained. Dr. Goldman did not revisit cognitive issues due to the comprehensive presentation given prior to his talk.
Results from a International Society for Pediatric Oncology (SIOP) study regarding participation in Clinical Trials
Clinical trials are not always available, however when these clinical trials are available they provide opinions from multiple doctors, may include central reviews, and include regimented treatments. This comprehensive approach may lead to less being missed. Dr. Goldman commented that new technology does not always mean the “new” approach is automatically better. He referenced proton beam therapy, stating that it certainly is cutting-edge and can be the preferred radiation treatment modality for some, not for all. Proton beam is particle therapy (using hydrogen that has been thrown and stripped of protons by an accelerator.) Another option, Intensity Modulated Radiation Therapy (IMRT) also has excellent control. Complimentary and alternative medicine were also briefly addressed. Complimentary approaches are not used instead of treatment, but to compliment. Alternative therapy differs from standard therapies and may differ from the treatment teams’ recommendations. It is advisable to have open dialogue with your treatment team. Palliative care addresses many issues, such as, emotional, social, spiritual, and physical. Vocational planning is critical to ensuring success for survivors.
Late Effects from treatments will be experienced by two thirds of survivors, physical and psychosocial. Dr. Goldman touched upon a wide variety of late effects. Some survivors will experience dental issues, lack of enamel, root thinning, teeth or roots that won’t grow. Ocular complications may include cataracts and may be steroid or radiation induced. Therapy would include removal of the cataract after the lesion impairs vision. Optic nerve atrophy is another complication for some patients. Hearing may be impacted by tumor, chemotherapy, and radiation. Frequent audiological exams, attention to dose modifications for toxic medications, cochlear implants, and audio rehabilitation are advisable for patients with hearing loss. Dr. Goldman provided a brief overview regarding fertility, thyroid, fatigue, secondary malignancies, central nervous system toxicities, cancer discrimination, and psycho-social issues that may affect survivors.
According to Dr. Goldman, the National Cancer Institute’s definition of a survivor states that survivorship issues begin at the time of diagnosis and continue through the rest of life.
In the afternoon, concurrent sessions were held. A brief summary is provided for two sessions.
Advances in Neuroimaging: Relevance for Diagnosis, Treatment and Identification of Recurrence, presented by Dr. Andrew Poet, University of Birmingham, The Birmingham Children’s Hospital

Dr. Poet provided an overview of progress made in imaging diagnostics for brain tumors. Imaging techniques are vital in the management of brain tumors for diagnostics, operative planning, post-operative assessment, monitoring during treatment, and follow-up. Over the past 50 years, diagnostics have improved in the advent of computerized tomography (CT), magnetic resonance imaging (MRI), but multiple other imaging modalities. Perfusion imaging provides information about blood vessels that help predict tumor response. Diffusion imaging indicates how solid a tumor may be, thus a predictor of progression. Functional imaging allows probing of the tumor. Other imaging options include metabolic imaging, quantitative imaging, magnetic resonance spectroscopy, and tractography.
Chemicals in tumors can predict outcome. Fats and lots of lipids predict tumors that do poorly. Looking at the edges of the tumor can predict outcome.
What’s on the horizon: Future of pediatric brain tumor treatment, presented by Maryam Fouladi, MD, Cincinnati Children’s, OH
Dr. Fouladi opened her talk by sharing the historical perspective of Avicenna, an 11th century physician, with an interest in ethics, whose beliefs at that time were that drugs must be pure, must be disease specific, time action must be observed, effect of drugs must be evidenced repeatedly, and trials must be done on humans, not just animals.
In present day, challenges include minimizing sequalae, discovering less toxic approaches, and finding successful targeted therapies.
Specific challenges noted:
Development of drugs: Finding biologically relevant target in tumor or microenvironment, looking at the pathway an environment, and the role in the disease process.
How to test?: The approach would be to study pre-clinical efficacy, pk anti-tumor targeted activity, mechanism of action, and biological activity, testing in adults first, then children in Phase I, II, and III clinical trials. Understanding tumor microenvironment and angiogenesis is critical for central nervous system tumors. A tumor is already 2 to 3 ml. in size when it will form new blood vessels to grow. The goal of treatment is to stop blood vessels from forming.
Dr. Fouladi provided an overview of various trials that are ongoing through the Children’s Oncology Group, Pediatric Brain Tumor Consortium, and CERN. Studies related to immunotherapy, oncolytic viruses, peptide vaccines for recurrent and newly diagnosed patients are being explored.

Other excellent topics were presented throughout the day, concurrently. This article only explores a sampling of some sessions. Young children were cared for and enjoyed games, arts and crafts, and a movie.
Written by Jeanne Young, President (excerpts taken from notes and presented slides).
CBTF was very pleased to be a strong supporter of the ISPNO and Nurses Symposium
