Eva Perdahl, MD, PhD, Children’s National-VA and David Wolf, MD, PhD, Johns Hopkins University
Brain tumors are the most common solid tumor of childhood. Among brain tumors, low-grade gliomas are the most common type, accounting for almost 50% of all tumor types.
There are two major types of cells that make up the brain: neurons and glia. Neurons are responsible for information processing. Glial cells are the support network for neurons. There are many types of glial cells, including astrocytes and oligodendroglia. Gliomas are tumors that arise from glial cells.
A tumor is called low-grade if it is slow growing and does not have the propensity to spread to other places or organs. On the WHO tumor grading scale, these are grade 1 or 2 tumors.
Types of Low-Grade Gliomas
There are many types of low-grade gliomas. They are classified by the appearance under the microscope or on their location. Some of the more common low grade gliomas are:
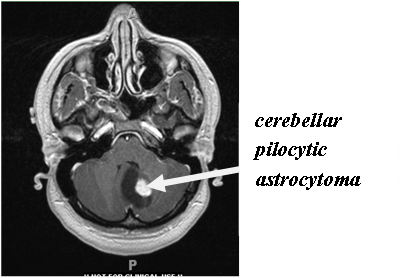
1. Pilocytic astrocytomas: These tumors are made up of astrocytes that have a spindle-like appearance (pilocytic). These are usually found in the cerebellum or hypothalamus. On imaging, they have a well-defined margin and do not cause swelling (edema).
2. Fibrillary astrocytomas: These tumors are made up of astrocytes that have fine fibers or filaments. These can occur in any part of the brain, and are often seen in the brainstem (midbrain). Unlike pilocytic astrocytomas, they tumors do not have a clear margin.
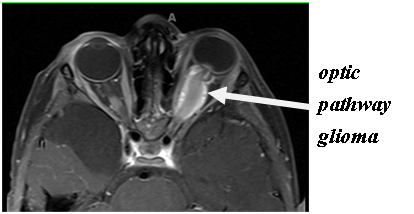
3. Optic pathway gliomas: These are pilocytic astrocytomas that arise from the optic nerve or optic pathway. This tumor is commonly associated with neurofibromatosis type 1.
4. Pleomorphic xathoastrocytoma: An astrocytoma that often has a cyst associated with it. It typically occurs in the temporal cortex.
5. Pilomyxoid astrocytoma: This is a subtype of pilocytic astrocytomas. It shows subtle differences under the microscope as compared to pilocytic astrocytomas. This tumor is more aggressive and has a greater potential to spread than pilocytic astrocytomas.
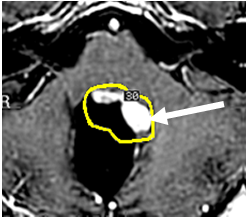
6. Subependymal giant cell astrocytoma (SEGA): This is a tumor seen in children with tuberous sclerosis. It occurs near the ventricles, and causes hydrocephalus.
Molecular Biology
We still do not know the cause of low-grade gliomas in children. A great deal of research to understand the molecular pathways that are involved in brain tumor development is ongoing. Work on the systems responsible for normal cell division has shown that a number of pathways in low grade gliomas are disrupted in ways that make cell division become uncontrolled. For example, aberrations in the mTOR pathway can lead to brain tumor formation. Everolimus, a drug that inhibits mTOR, has been shown to be an effective therapy subependymal giant cell astrocytomas. Clinical trials using everolimus in other types of low grade gliomas are currently underway.
Another exciting area involves RAF kinases. This system controls cell proliferation and cell death. Mutations in BRAF, a specific RAF kinase, appear to be an important factor in the development of pilocytic astrocytomas. An antibody against this mutated protein is already in use for patients with metastatic melanoma. Methods for identifying the BRAF mutation are still not standardized or readily available for general clinical use at this time.
Symptoms
The symptoms caused by low-grade gliomas are dependent on the location of the tumor. Children with a pilocytic astrocytoma in the cerebellum will have headaches, nausea and vomiting, poor coordination and difficulty walking (ataxia). Tumors found in the cortex, such as pleomorphic xanthoastrocytomas, often cause seizures or weakness in the arms or legs. Hypothalamic astrocytomas can cause problems with hormone function, such as early puberty or problems with vision. Optic pathway gliomas can cause vision loss, lazy eye (strabismus), or bulging of the eye (proptosis).
Treatment options
The treatment of low-grade glioma primarily depends on the location of the tumor and age of the child. Not all low-grade gliomas require treatment; tumors that are not causing symptoms are often simply followed closely.
1. Surgery: The goal of surgery is to remove (resect) as much of the tumor as possible without damaging normal brain tissue. If neurosurgeon feels the tumor is in a location where the likelihood of unacceptable side effects (paralysis, vision loss), then a small piece of the tumor is obtained to confirm the diagnosis (biopsy). Pilocytic astrocytomas in the cerebellum or pleomorphic xanthoastrocytomas can often be completely removed by surgery. On the other hand, fibrillary astrocytomas are harder to completely remove with surgery, and are typically diagnosed with a biopsy alone. Low-grade gliomas that are completely removed often do not require any additional therapies.
2. Radiation therapy: Radiation therapy is a very effective treatment of brain tumors. In older children, when the glioma cannot be fully removed, it is typically the first choice of therapy. Radiation oncologists manage this type of therapy, and they have a number of techniques available. Radiation therapy is not commonly used in younger children due to its significant effect on brain development.
3. Chemotherapy: Chemotherapy is used to stop tumor growth or shrink the tumor. It is often utilized to delay the time before giving radiation therapy (in younger children). There are multiple types of effective chemotherapies available. Some are given intravenously and others are pills. Some are given on a weekly or even monthly basis. Chemotherapy is managed by an oncologist.
Some children with low-grade gliomas requiring treatment are enrolled in clinical trials to help us learn how well new medications are tolerated, if there are better ways to treat these tumors, or to reduce side effects and long term complications. Cinical trials may involve any of the above treatment options.
Prognosis
The overall prognosis for children with low-grade gliomas is excellent, with 90% of children alive at 5 years. Long-term effects depend on the location of the tumor and the type of treatment used ( in the case of radiation, the age of the patient at time of treatment as well). For children with tumors in the hypothalamus, hormone deficiencies, particularly related to salt balance, may be permanent. However, they can be treated with daily medication. Vision loss can stabilize with tumor treatment, but typically does not improve. Seizures can be cured following complete removal of the tumor.
Updated by David Wolf, MD, PhD, original article by Eva Perdahl, M.D., Ph.D., Children’s National-VA
Revised and updated by David Wolf, MD, PhD, Johns Hopkins University – April 6, 2012

 My daughter is a true success story!
My daughter is a true success story!